|
The principal role of the reproductive system is to assure the continuation of the human species. Other systems in the body, such as the endocrine and urinary systems, work continuously to sustain a balance in the body for the survival of the individual. People may live a healthy, long, and happy life without producing offspring, but if the species is to remain, at least some people must have children.
In the case of conceiving children, the reproductive system has four primary functions:
- Production of egg and sperm cells
- Transport and sustain the egg and sperm cells
- Nurture the developing offspring
- Production of hormones
The primary reproductive organs, or gonads, consist of the ovaries and testes. These organs provide the egg, sperm, and hormones. The hormones aid in the regulation of the physiology, maturation, and the managment of the reproductive system
Does Everyone Have the Same Reproductive Anatomy?
Most people have either a vulva or a penis and a scrotum; however, everyone’s sexual anatomy is a bit different. When an infant is born, the doctor most likely assigns a sex of male or female—based on the physical anatomy. The assigned sex doesn’t necessarily say anything about the person’s identity.
Some individual’s assigned gender and assigned sex are pretty much the same, or in line with each other—these people are known as cisgender. Other people feel that the sex identity they were assigned at birth doesn’t suit their gender identity. For example, an individual could be born with a penis, assigned male as a baby, but later identifies as a female. These people often call themselves transgender.
No matter if you are a medical scribe, a health-care professional, or someone interested in reproductive biology, it is important to understand that some sex anatomies don’t fit the conventional definition of female or male—these individuals may be described as intersex. There are many combinations of body parts and hormones that fall under the intersex umbrella. Being intersex doesn’t signify any connection with an individual’s gender identity.
Male Reproductive System
The male reproductive system, like that of the female, consists of organs whose purpose is to achieve reproduction. This system consists of:
- Testes
- A system of excretory ducts,
- Seminal vesicles
- The prostate
- The bulbourethral glands
- The penis
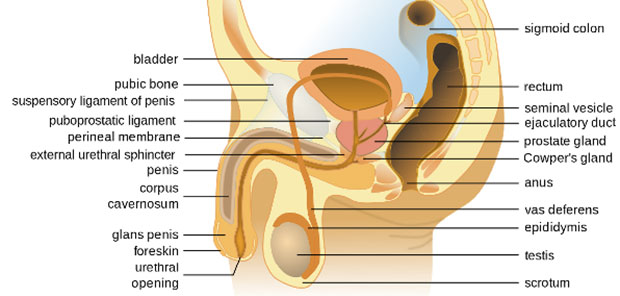
Testes
The male gonads, also known as testes or testicles, begin to develop in the abdominal cavity, up near the kidneys. During the eight weeks just before birth, or shortly after birth, the testes descend into the scrotum through the inguinal canal. The scrotum is a pouch that is below the abdomen and posterior to the penis. Although this location of the testes may seem to make them vulnerable to injury, it provides a temperature about 3° C/37.4° F below the average body temperature. This lower temperature is essential for the production of viable sperm, spermatogenesis. In addition, the gonads are responsible for male hormone production.
The scrotum consists of skin, which is the outer layer, and subcutaneous tissue, the layer under the skin. A vertical septum, or wall, of subcutaneous tissue divides the scrotum into two parts—each part contains one testicle. Smooth muscle fibers, called the dartos muscle, within the scrotum contract to give the scrotum its wrinkled appearance. When the muscle fibers are relaxed, the scrotum’s appearance is smooth. Another muscle, the cremaster muscle, consists of skeletal muscle fibers—this controls the location of the scrotum and testes. When a man is cold or sexually aroused the muscles contract to pull the testes closer to the body for warmth.
Excretory Duct System
Sperm cells move through a series of ducts to reach the outside of the body. After the sperm cells leave the gonads, the sperm pass through the:
- epididymis,
- ductus deferens,
- ejaculatory duct, and
- the urethra.
Epididymis
Sperm exists the testes through efferent ducts that enter each of the epididymides. The epididymides are tubes about 6 meters long that tightly coil to form a comma-shaped organ—they are located along the upper back margins of the testes. When the sperm leaves the testes, they are immature, inadequate, and not able to fertilize an ova. They complete their maturation process as they move through the epididymis. Mature sperm, capable of fertilization, are stored in the lower part, or tail, of the epididymis.
Ductus Deferens
The vas deferens, also known as the ductus deferens, is a tube that shares a common border with the epididymis. It begins at the bottom, or tail, of the epididymis, then curves upward along the back margin of the testes. The ductus deferens travels through the abdominopelvic cavity where it crosses over the posterior portion of the bladder, and then it descends along the back wall of the bladder toward the prostate gland.
Before each ductus deferens reaches the prostate gland, they enlarge to form an ampulla, or reservoir. Sperm is then stored in the proximal portion of the ductus deferens, closest to the center of the body, near the epididymis. Peristaltic movements, which is an involuntary contraction and relaxation of the ductus deferens, propel the sperm through the tube.
Ejaculatory Duct
At the ampulla, each ductus deferens joins the duct from one of the accessory glands, the adjacent seminal vesicle, to form a short ejaculatory duct. The ejaculatory ducts pass through the prostate gland and empty into the urethra.
Urethra
The urethra extends from the urinary bladder to the external opening at the tip of the penis, known as the urethral orifice. It is a passageway for fluids and sperm from the urinary system and the reproductive system. Sphincters contract tightly to keep urine from entering the urethra while reproductive fluids are passing through the urethra.
Seminal Vesicles
The two seminal vesicles are posterior to the urinary bladder—each gland has a small duct that connects with the ductus deferens at the ampulla to form an ejaculatory duct, which then empties into the urethra. The fluid from the glands is thick and contains fructose, which is a source of energy for the sperm; prostaglandins, which aid to the movement and viability of the sperm; and proteins that cause a slight coagulation reaction, changing the liquid to a semi-solid state, in the semen after ejaculation.
Prostate
The prostate gland is a dense structure about the size of a walnut that is located just behind the urinary bladder and encircles the urethra as it leaves the urinary bladder. Secretions of the prostate enhance the motility of the sperm. The secretions are alkaline, thin, and milky in color.
Bulbourethral Glands
The paired Cowper’s glands, known as the bulbourethral glands, are about the size of a pea—located near the base of the penis. During sexual stimulation, the bulbourethral glands secrete a mucus-like fluid. This alkaline fluid neutralizes the acidic urine residue in the urethra, provides some lubrication for the tip of the penis, and helps to neutralize the acidity of the vagina.
Seminal Fluid
Seminal fluid, or semen, is slightly alkaline. It is made up of approximately 60 % of fluid from the seminal vesicles and the remainder coming from the prostate gland. Only a small volume is from the bulbourethral gland.
In a single ejaculation, the amount of sperm varies from 1.5 to 6.0 mL—containing between 20 to 150 million sperm per mL. Although only one sperm will penetrate and fertilize the ovum, or egg, it takes several million sperm in one ejaculation for the fertilization to take place. Fertility issues arise when sperm counts are below 10 to 20 million.
Penis
The penis, a copulatory organ, is a round pendant organ located in front of the scrotum—its function is to transfer sperm to the vagina during sexual intercourse. The penis has three columns of erectile tissue: two dorsal columns, on the top side of the penis, called the corpora cavernosa and a single ventral column that surrounds the urethra on the bottom side of the penis called the corpus spongiosum. The columns are encircled with connective tissue and covered with skin.
Male Reproductive Hormones
The male sexual response includes erection, orgasm, and the ejaculation of semen. After an orgasm, there is a period during which the male cannot achieve another erection—this time period is variable.
Three principle regulators of the male reproductive system are the:
- follicle-stimulating hormone (FSH), stimulates spermatogenesis;
- luteinizing hormone (LH), stimulates the production of testosterone; and
- testosterone, stimulates the development of male secondary sex characteristics and spermatogenesis.
Female Reproductive System
The female reproductive system’s role is to produce female sex hormones, sustain egg cells, or ova, transport ova for fertilization by the sperm, provide a viable environment for a developing fetus, and move the fetus to the outside world after the development period.
The female reproductive system includes the:
- Ovaries
- Fallopian tubes
- Uterus
- Vagina
- External genitalia
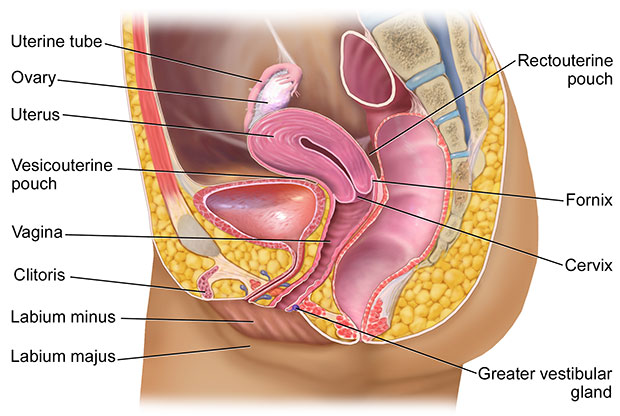
Ovaries
The two ovaries, or female gonads, are the primary female reproductive organs. Each ovary has a dense, ovoid structure about the size and shape of an almond. The ovaries are protected in the ovarian fossa, which are shallow depressions on each side of the uterus near the side walls of the pelvic cavity—they are held in place by peritoneal ligaments.
A layer of epithelium covers the ovaries called the germinal epithelium. Underneath this outer layer of cells is the tunica albuginea, which is a capsule of connective tissue—this is divided into an outer cortex and an inner medulla.
- The outer cortex has many ovarian follicles that assist in various stages of development. Each of the follicles has an oocyte, a female germ cell that is an immature egg. A germ cell contains half the number of chromosomes (23 chromosomes) that is needed to create offspring. The two germ cells that complete one another are the egg and the sperm for a total of 46 chromosomes.
- The inner medulla is connective tissue with ample blood vessels, lymphatic vessels, and nerve fibers.
Oogenesis
Gametes, or female sex cells, develop in the ovaries by oogenesis, which is called meiosis. Oogenesis is similar to spermatogenesis.
- Primitive germ cells in early in fetal development differentiate into oogonia (46 chromosomes)—these divide to form thousands of cells, still called oogonia.
- After a growth phase, the oogonia become primary oocytes (46 chromosomes) that then replicate their DNA and begin the first meiotic division, meiosis I—this process is suspended in this state until puberty.
- Beginning at puberty, under the influence of FSH, several primary oocytes start to grow each month.
- One of the primary oocytes outgrows the others, and it resumes meiosis I to become a secondary oocyte (23 chromosomes). The other cells degenerate. An in-depth description is found here.
The two ovaries together contain about 700,000 oocytes at birth—this is a lifetime supply, and no more will develop. This differs from the male in which spermatogenesis continues to be produced throughout the reproductive life. By puberty, the amount of primary oocytes has further declined to about 400,000.
Fallopian Tubes
The fallopian tubes are very fine tubes that eggs travel to get from the ovaries to the uterus during ovulation. The mature egg is released from the ovary, pushed through the fallopian tube, and is made available to be fertilized by sperm.
Approximately every month, or about every 21 to 45 days, an egg will mature within one of the ovaries. As it reaches full development, the egg is released by the ovary where it enters into the fallopian tube to make its way to the uterus to wait for sperm.
The lining of the uterus has prepared for a fertilized egg by thickening. If no conception occurs, the uterine lining is sloughed off. The shedding of the uterine wall and the unfertilized egg is known as menstruation.
Uterus
The uterus is a muscular organ that the fertilized oocyte travels to from the ovary through the fallopian tube—it provides a suitable environment for the developing fetus. Before the first pregnancy, the uterus is about the size and shape of a pear, with the narrow portion directed inferiorly. After childbirth, the uterus is usually bigger, then reverts to a smaller size after menopause.
The uterus is lined with endometrium, which is a glandular mucous membrane. The stratum functionalis of the endometrium is what sloughs off during menstruation. The deeper stratum basale is a foundation for rebuilding the stratum functionalis.
Vagina
The vagina, a fibromuscular tube that extends from the cervix of the uterus to the outside of the body—located between the rectum and the urinary bladder. The cervix projects into the vagina at almost a right angle. The vagina serves as a passageway for menstrual flow, receives the erect penis during intercourse, and is the birth canal during childbirth.
External Genitalia
The accessory structures of the female reproductive system are external to the vagina. The external genitalia is also referred to as the vulva. The vulva includes the:
- mons pubis,
- labia majora,
- labia minora,
- clitoris, and
- vestibule glands.
Similar to the penis, the clitorisis an erectile organ that responds to sexual stimulation. Posterior to the clitoris, the urethra, vagina, paraurethral glands, and greater vestibular glands open into the vestibule.
Female Reproductive Hormones
The female sexual response involves arousal and orgasm. Unlike the male sexual response, there is no ejaculation. An egg is capable of fertilization without the female having an orgasm.
The following hormones have major roles in the female reproductive system:
- Follicle-stimulating hormone
- luteinizing hormone
- estrogen
- progesterone
When a female’s ovaries and uterus are mature enough to respond to hormonal stimulation, such as in puberty, certain stimuli cause the hypothalamus, the master switchboard of the endocrine system, to start producing and secreting gonadotropin-releasing hormone. This hormone travels to the anterior pituitary gland, the master gland, where it stimulates the secretion of follicle-stimulating hormone and luteinizing hormone. Both hormones, in turn, affect the ovaries and uterus and create the female monthly cycle. Monthly reproductive cycles last from menarche, the start of a woman’s menstruation, to menopause.
The ovarian and the uterine cycle take place simultaneously.
The monthly ovarian cycle:
- begins with the follicular phase—follicle development;
- continues with the ovulatory phase; and
- concludes with the luteal phase.
The monthly uterine cycle:
- starts with the menstrual phase;
- continues with the proliferative phase—repair of the endometrium; and
- ends with the secretory phase—growth of glands and blood vessels.
Menopause occurs when the reproductive cycles cease. This period is characterized by reduced levels of ovarian hormones and elevated follicle-stimulating hormone and luteinizing hormone. The alteration in hormone levels is responsible for the symptoms women have during menopause.
Click here for more Information.
|